Although anyone can contract COVID-19, endemic racism, insurance disparity and job conditions make the contagious rate higher for vulnerable people of color.
As the novel coronavirus continues its rapid spread across the nation, advocates, lawmakers and public health experts have sounded the alarm on the devastating impact the virus can have among Blacks, Latinos and Native Americans. The reason for this goes back to a basic racial divide in the U.S. that the COVID-19 crisis has brought to the surface.
That’s because although anyone can be infected with COVID-19, recent studies show that the virus can impact the poor, the vulnerable, the marginalized and communities of color -who sometimes live in densely populated inner cities- in larger numbers. And it’s not that people of color are necessarily more vulnerable to getting coronavirus, but that they’re more vulnerable to being exposed to it and having more severe manifestations when they contract it, which can lead to hospitalization and death. Poverty and a lack of access to quality health care, insurance, vital resources and underlying health conditions are to blame.
RELATED: It’s Census Day. Here’s How Stacey Abrams’s Fair Count Is Fighting to Ensure Black Men Are Counted.
A Problem Long Before COVID-19
The National Institute of Allergies and Infectious Diseases (NIAID) has long recognized that racial and ethnic differences affect susceptibility to infection and disease, and the numbers bear it out. To cite some examples, people with asthma have a higher risk of suffering complications from COVID-19. And according to the latest numbers available, approximately 2.2 million Hispanics/Latinos in the United States report having asthma, with Puerto Rican Americans having almost three times the asthma rate of the overall Hispanic population. African American women, on the other hand, are 20% more likely to have asthma than non-Hispanic whites.
Another study shows that African Americans were 60% more likely to be diagnosed with diabetes and twice as likely as non-white Hispanics to die from it, while American Indians/Alaska Natives were three times more likely to have diabetes and 2.5 times more likely to die from it, according to the Federal Department of Health and Human Services Office of Minority Health. But underlying medical conditions are just one side of the story.
RELATED: Landmark Legislation Seeks to Reduce Black Maternal Health Risks
Endemic Racism
“Structural and environmental racism” also contribute to the high incidence of underlying or chronic health conditions in people of color, says The Center for American Progress, a public policy research and advocacy organization with headquarters in Washington, D.C.
The highest number of uninsured people in the United States are Latinos at 17.8%, while only 5.9% percent of White Americans are uninsured, says Salud America!, a national Latino-focused advocacy organization of the Institute for Health Promotion Research (IHPR) at UT Health San Antonio, Texas. The result of this disparity is families that must often choose between paying rent and putting food on the table or getting routine checkups and seeking medical care.
In Chicago, for example, 72% of the deaths caused by COVID-19 have been among the city’s black residents, though they make up 29% of the population, and the numbers are almost identical in Louisiana.
RELATED: Less Than 16% Of Latinos Can Actually Work From Home
For its part, Florida has over 100,000 immigrant farm workers, mainly from Mexico and South and Central America, according to the Department of Housing and Urban Development (HUD). But the men and women who work the fields often lack health insurance and fail to seek medical care, which makes them more vulnerable to COVID-19. And Hialeah, the sixth-most populous municipality in the state, could become a hot zone for the virus not only for the fast growing number of cases, but because of the city’s large senior citizen population, a majority of whom live in assisted living facilities, nursing homes, public housing projects and rentals subsidized with Section 8 vouchers.
People of color could also be more at risk of contracting the disease because of their professions, such as construction, retail, housecleaning, health care, home care aid or any job that can’t be done from home. Add to this having a language barrier or the need to take public transportation to go to and from work, and it’s clear why communities of color remain the most vulnerable in the midst of the pandemic.
He said what? 10 things to know about RFK Jr.
The Kennedy family has long been considered “Democratic royalty.” But Robert F. Kennedy, Jr.—son of Robert F. Kennedy, who was assassinated while...

Here’s everything you need to know about this month’s Mercury retrograde
Does everything in your life feel a little more chaotic than usual? Or do you feel like misunderstandings are cropping up more frequently than they...
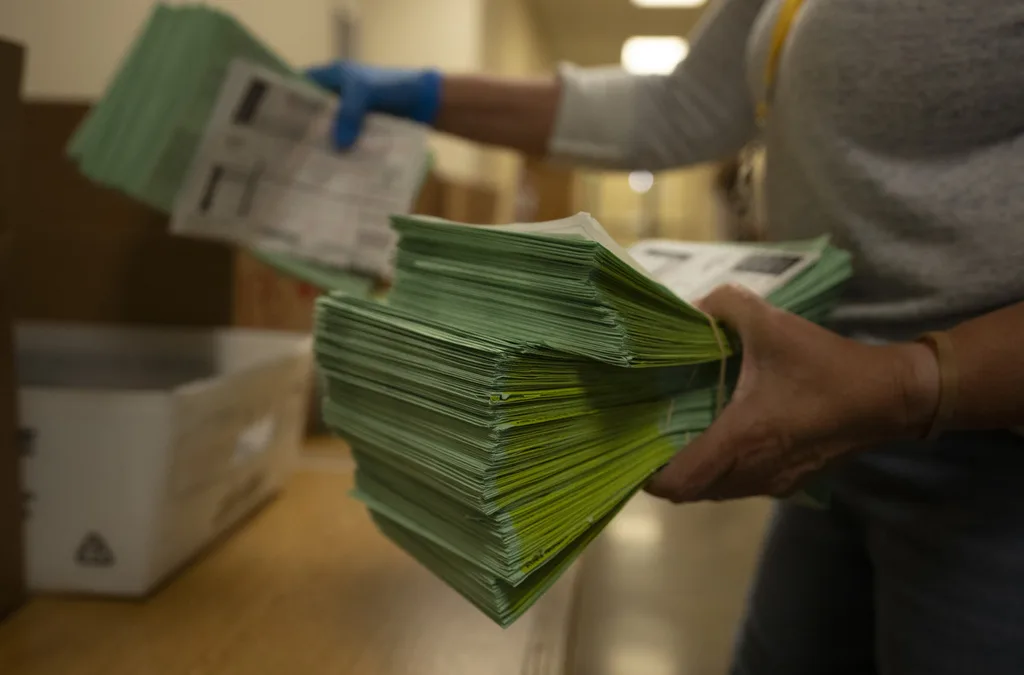
Arizona expects to be back at the center of election attacks. Its officials are going on offense
Republican Richer and Democrat Fontes are taking more aggressive steps than ever to rebuild trust with voters, knock down disinformation, and...

George Santos’ former treasurer running attack ads in Arizona with Dem-sounding PAC name
An unregistered, Republican-run political action committee from Texas with a deceptively Democratic name and ties to disgraced US Rep. George Santos...